Why Does Flu Have a Season?
by Felix Horns
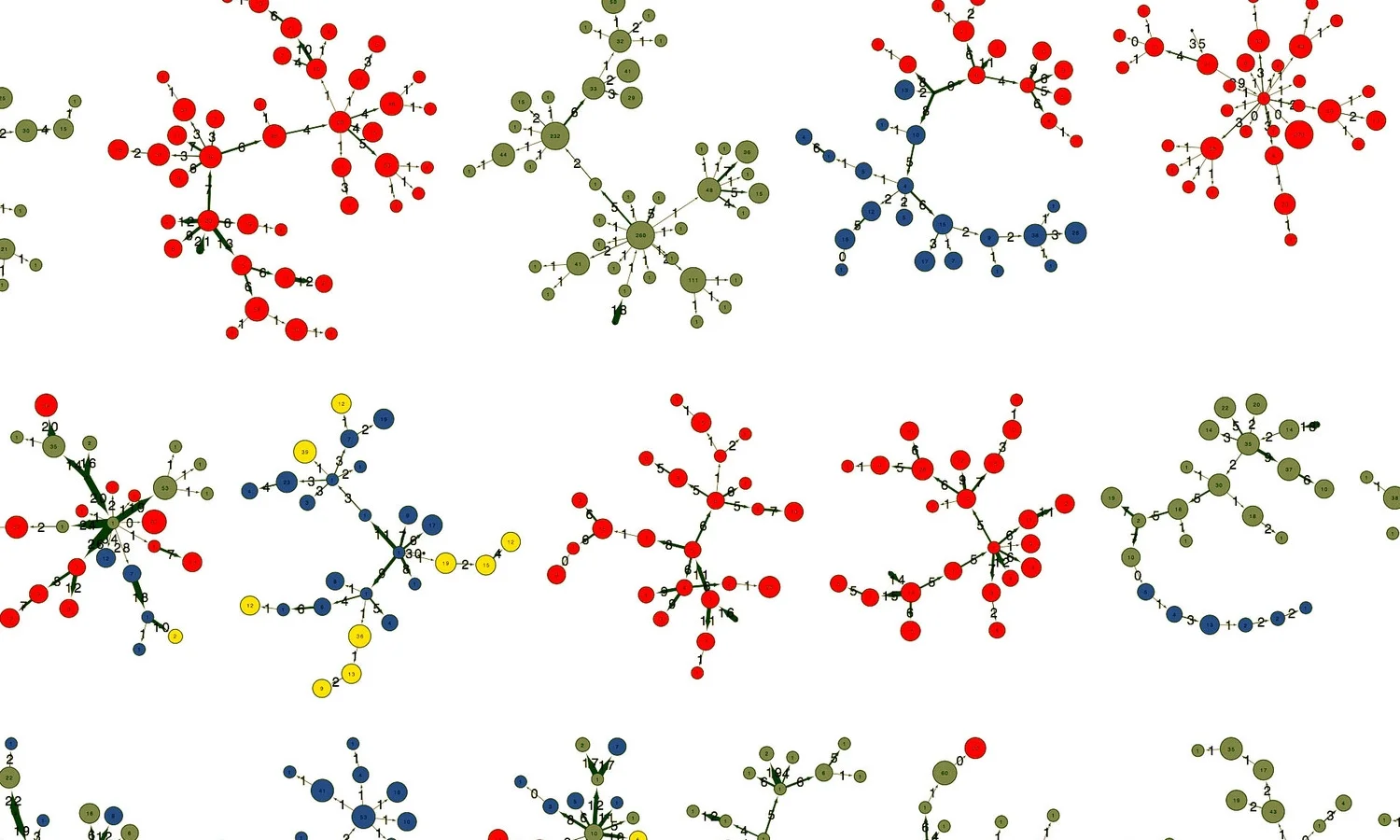
Flu antibodies in a single blood sample: your body's immune defense against influenza. These antibodies have been sorted into families, and as you can see, hundreds of lineages are found in a single drop of blood.
Fall is a time of ritual. Around the globe, societies celebrate the season with harvest feasts and quirky traditions, from moon cakes and floating lanterns in China to turkey and American football in the USA. In temperate regions, flu is another autumn tradition, albeit a less savory one.
In the West, one in four catches influenza each year, incapacitating millions with aches and fevers, and costing an estimated $100 billion in treatment expenses and sick days. And for infants and the elderly, flu can be deadly. The World Health Organization estimates that flu kills a quarter to a half million people every year worldwide.
Flu shots offer tantalizing relief: protection from each year’s unique strain of influenza virus.
But Influenza evolves fast. It is locked in an evolutionary arms race with our immune systems, ever-mutating to escape its host’s defenses. Because flu changes so quickly, it is effectively a new disease every year. That’s why we can catch it many times throughout our lives and why we need a new flu shot every autumn.
Immunization reduces the scope of the annual flu epidemic, but doesn’t prevent it entirely. Despite the existence of vaccines, flu season unfolds from autumn into winter, beginning in October and peaking in January.
Why does flu peak in winter? Surprisingly, answers to this simple question have only begun to emerge in the past 5 years. To parents and teachers, wranglers of runny-nosed, toy-chewing children, it will come as no surprise that one of the leading theories blames back-to-school season for the yearly flu epidemic.
Over summer, kids frolic at summer camps and roam the streets of sun-drenched neighborhoods. Come September, they go back to school, into classrooms full of new faces, new friends, and new germs. Each kid brings his or her own infections to school, which spread like wildfire through naïve immune systems. The children exchange never-before-seen bugs, which their bodies are not primed to fight.
Schools become cesspools of disease. Infections trickle onward to parents, siblings, and the rest of society.
Although this idea has never been directly tested for flu, scientists have found support for the schools-as-cesspools hypothesis in measles, which is caused by another highly contagious virus.
For much of history measles, which causes a distinctive maroon rash, was ubiquitous. As Babbott and Gordon put it, measles was “as inevitable as death and taxes.” Nearly every child caught it by the time they were 15, until the disease was eliminated from the developed world by vaccines in the late 1960s.
Records of measles infections between 1944 and 1966 reveal the movement of outbreaks across England. Major epidemics often struck Cambridge two weeks after the nearby metropolis of London. In the northwestern industrial centers of Manchester and Liverpool, distinct epidemics spread outward to neighboring towns. For much of the 20th century, measles manifested as seasonal waves of disease sweeping out from large urban centers to surrounding hinterlands, revealing the flow of people and viruses in space and time.
Those records of measles infections show an annual or biennial spike in measles coinciding with children returning to the classroom in autumn. What’s more, measles outbreaks tracked birth rates.
Four or five years after a baby boom, a huge crop of new kindergarteners entered the English school system. Measles spread quickly without resistance from their naïve immune systems, triggering an epidemic.
When analyzed this way, birth rates predict measles epidemics, supporting a key role for schoolchildren in spreading the disease.
But measles is a simpler disease than flu. Like chicken pox, measles is most common in children, and only strikes once before the body develops long-lasting immunity. However, unlike measles, influenza virus evolves fast. Its tremendous genetic variation enables the flu to evade our immune systems and infect us again every year.
The cold, dry weather of winter also seems to play an important role in the timing of the annual flu epidemic. Influenza virus survives better in air and on surfaces when temperature and humidity are low, so it transmits from person to person more easily.
To make matters worse, the layer of mucus in your airway is your first line of defense against respiratory bugs, trapping and clearing unwelcome viruses. Low temperatures and humidity make mucus more viscous, so it removes viruses less effectively. Consistent with this, winter flu epidemics in the northeastern USA often occur in weeks after sharp drops in humidity.
While the weather seems to influence the timing of flu epidemics, schoolchildren are likely another key piece in the puzzle.
Children come into close contact in the schoolyard every day. Scientists tracking the spread of flu have found that parents living with school-age children are at increased risk of catching the flu themselves. And the risk is even higher if you live with preschoolers. As you might predict, school holidays cut flu transmission by one quarter.
We are beginning to understand the causes of annual flu epidemics, but cannot yet abolish them. Since influenza relies on schoolchildren, we may be able to hamstring the virus by vaccinating kids, and the parents and teachers who contact them.
But to develop effective vaccines, we need a better understanding of how influenza virus evolves. Every year, the world’s top infectious disease scientists and policymakers gather to predict which strains of flu will be most common. If they can predict the most common strains, then the flu vaccine will work well. But they only get it right half the time.
Why? Because we don't understand how the flu virus evolves.
Each year, one strain of the virus is most common. As it evolves, the virus gives rise to many hundreds of slightly different progeny. It’s hard to predict which strain will be successful in the next year. Influenza is one cold-weather tradition that we could do without; an understanding of how flu spreads and evolves will bring us closer to that end.
Felix Horns is a graduate student in Biophysics at Stanford University, working on immune health. He can be reached at rfhorns@stanford.edu